Introduction
While the aspiration of a foreign body is rarely seen in adults, it is a frequent and serious condition in children as mentioned by Oztuna et al (2005). The most common cause of endobronchial foreign bodies is the aspiration of oropharyngeal material into the lower respiratory tract. It is, however, also possible for foreign bodies from an extrapulmonary site to migrate to the endobronchial space. In a study by Haddad et al (2004) it is stated that gauze, towels, sponges and surgical instruments are rarely left in the thoracic cavity or mediastinum postoperatively, especially after a pneumonectomy. It is also very uncommon for a gauze to be retained at mediastinoscopy or video-assisted mediastinoscopic lymphadenectomy (VAMLA). We present a case that had a prior VAMLA and pneumonectomy, expectorating a gauze which had been forgotten in the mediastinum and had migrated into the trachea.
Case Report
A 57-year-old man had a staging radical video-assisted mediastinoscopic lymphadenectomy (VAMLA) mediastinoscopy and right-sided pneumonectomy for squamous cell lung carcinoma two years ago. A month later, postoperative control fiberoptic bronchoscopy (FOB) revealed a mucosal bulging on the distal portion of his trachea. Biopsy was negative for tumour cells. Postoperative 2nd year control thorax computed tomography (CT) showed a polipoid nodular opacity protruding into distal trachea. A biopsy was taken via FOB from the lesion, which was reported as mixed inflammatory infiltrate composed of leucocytes, lymphocytes, histiocytic giant cells and commented to be a ‘benign polipoid nodule’. Then this 0.7 x 0.7 cm lesion was removed with snare and cauterised with argon plasma during another FOB session.
Three months later, the patient stated that he was coughing up foul smelling sputum. Another bronchoscopic biopsy was conducted and ‘squamous metaplasia and histiocytic giant cells with foreign bodies (suspected suture material) within their cytoplasms’ were reported by our colleagues in pathology department. There was a 19 mm density with air loculations at the right anterior lateral side of his distal trachea in thorax CT (Fig. 1).
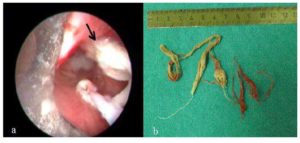
The patient told us about expectorating strange, cloth-like substances. Rigid bronchoscopy was conducted. Gauze was protruding from right tracheobronchial angle and moving with respiration (Fig. 2a). It was removed completely using a rat tooth with alligator jaws’ type grasping forceps (Fig. 2b).
Control FOB after 10 days revealed that defect area, which the foreign body was extracted from, was almost fully healed.
The patient was relieved of constant coughing and he is still healthy with no problems after three years since pneumonectomy and 13 months since removal of the retained gauze.
Discussion
VAMLA is a technique developed for exact pretherapeutic lymph node staging of lung cancer that was first described by Hürtgen and colleagues (2002). We have been using it successfully since 2004 with satisfactory results.
We think that the retained gauze was from VAMLA and it was forgotten in the left lower paratracheal area. A minor bleeding from 4L localization which stopped with compression is documented in our operative records. Although the gauze was retrieved from the right side, no clues suggesting a foreign body was evident during his right pneumonectomy. This particular case had an average of 6cc lymphatic tissue dissected per station in VAMLA. Lymph node stations 2R, 3, 4R, 7, 9R and 10R were dissected during thoracotomy and no sign of a foreign body was present.
In our clinic practice, gauzes used in VAMLA are rolled and cut smaller than the ones used in a thoracotomy. So, it was easy to recognize that it was from the previous VAMLA.
Also, a right sided foreign body in a patient with right pneumonectomy would have likely migrated into the postpneumonectomy cavity or mediastinum rather than trachea during a period of two years.
As Topal et al (2001) mentioned, in a patient with the history of surgery, biopsy findings of fibers obviously should alert the physician to the presence of a retained sponge.
Sometimes, the desire for more lymph node dissection to achieve better staging results tends to lead the surgeon to pursue a more aggressive approach in VAMLA. While this ensures low false negative results in staging, it increases the risk for bleeding and associated complications.

Figure1: Postoperative control Thorax CT
Figure 2: Foreign body extraction via rigid bronchoscopy (a). Black arrow shows the tracheal defect area. Removed gauze (b)
References
1. Haddad R, Judice LF, Chibante A and Ferraz D. (2004) ‘Migration of surgical sponge retained at mediastinoscopy into the trachea,’ Interactive Cardiovascular and Thoracic Surgery, 3 (4) 637-640.
Publisher – Google Scholar
2. Hürtgen M, Friedel G, Toomes H and Fritz P. (2002) ‘Radical video-assisted mediastinoscopic lymphadenectomy (VAMLA) technique and first results,’ European Journal of Cardiothoracic Surgery, 21 (2) 348-351.
Publisher – Google Scholar
3. Oztuna F, Bülbül Y and Ozlü T. (2005) ‘An unusual endobronchial foreign body: a gauze that migrated from the mediastinum,’ Respiration, 72 (5) 543.
Publisher – Google Scholar
4. Topal U, Gebitekin C and Tuncel E. (2001) ‘Intrathoracic gossypiboma,’ American Journal of Roentgenology, 177 (6) 1485-1486.
Publisher – Google Scholar