Therefore, the novality of this research is that it combines the rigidity of chrome-cobalt skeleton partial denture framework with its good support and better load distribution, together with the superior esthetic quality of the thermoelastic (Versacryl) retentive arm. Another important advantage of the thermoelastic retentive arm is that it has an internal memory to return to its original position as compared to the cast clasp, which usually becomes fatigued after about 500 times of insertion and removal, as reported by Tokue et al (2013).
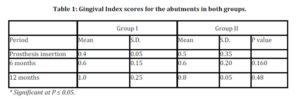
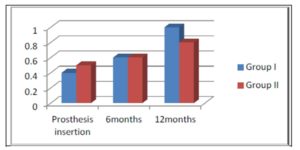
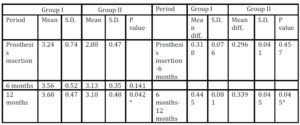
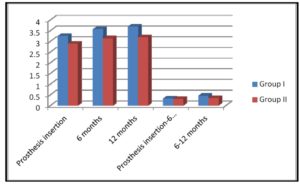
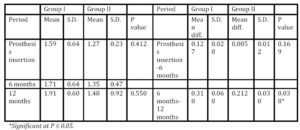
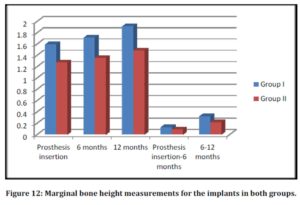
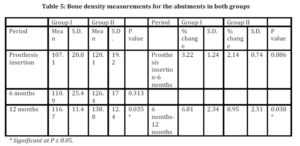
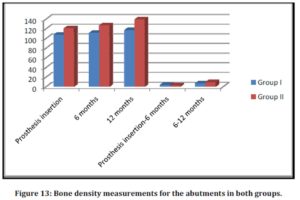
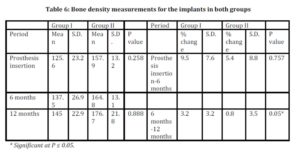
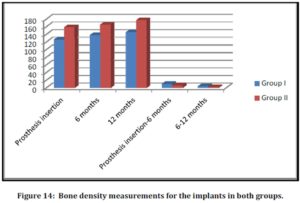
The present study revealed superior results regarding the amount of bone loss, density and gingival condition around the terminal abutment, and implant with the use of the thermoelastic resin (Versacryl) clasp. Besides, this type of clasp arm can be easily adjusted by just putting it in warm water which gives confidence and comfort to the patient, unlike the metal clasp arm. Another important advantage of the Versacryl clasp is that, if broken, it can be easily replaced, as it chemically bonds to the old acrylic resin. In addition, thermoelastic resin clasps are also very hygienic and do not easily stain as they are non-porous and easily cleaned preventing the adherence of debris to the clasp.
Conclusions
From the results of the present study, it can be concluded that:
1) The use of the thermoelastic (Versacryl) clasp, with its superior properties, is better accepted by the patients, regarding esthetics, retention and efficiency.
2) Both the implants and the abutment teeth reacted more favorably with the use of Versacryl clasps
References
1) Behr M, Zeman F, Passauer T, Koller M, Hahnel S, Buergers R, Lang R, Handel G and Kolbeck C (2012) “Clinical performance of cast clasp-retained removable partial dentures: a retrospective study,” International Journal of Prosthodontics, 25(2):138-144.
Google Scholar
2) Budtz-Jørgensen E, Bochet G, Grundman M and Borgis S (2000) “Aesthetic considerations for the treatment of partially edentulous patients with removable dentures,” Practical Periodontics and Aesthetic Dentistry, 12(8):765-772.
Google Scholar
3) Chikunov I, Doan P and Vahidi F (2008) “Implant-retained partial overdenture with resilient attachments,” Journal of Prosthodontics, 17(2):141-148.
Publisher – Google Scholar
4) de Freitas RF, de Carvalho Dias K, da Fonte Porto Carreiro A, Barbosa GA and Ferreira MA (2012) “Mandibular implant-supported removable partial denture with distal extension: a systematic review,” Journal of Oral Rehabilitation, 39(10):791-798.
Publisher – Google Scholar
5) El Mekawy NH, El-Negoly SA, Grawish Mel-A and El-Hawary YM (2012) “Intracoronal mandibular Kennedy Class I implant-tooth supported removable partial overdenture: a 2-year multicenter prospective study,” International Journal of Oral and Maxillofacial Implants, 27(3): 677-683.
Google Scholar
6) Elsyad MA and Habib AA (2011) “Implant-supported versus implant-retained distal extension mandibular partial overdentures and residual ridge resorption: a 5-year retrospective radiographic study in men,” International Journal of Prosthodontics, 24(4):306-313.
Google Scholar
7) Hamanaka I , Takahashi Y and Shimizu H (2011) “Mechanical properties of injection-molded thermoplastic denture base resins,” Acta Odontologica Scandinavica. 69:75—79.
Publisher – Google Scholar
8) Ito M (2013) “The combination of a nylon and traditional partial removable dental prosthesis for improved esthetics: A clinical report,” Journal of Prosthetic Dentistry, 109(1): 5-8.
Publisher – Google Scholar
9) Jivraj S and Chee W (2006) “Treatment planning of implants in posterior quadrants,” British Dental Journal, 201(1):13-23.
Publisher – Google Scholar
10) Kaplan P (2012) “Flexible partial denture variations. The use of circumferential, combination, and continuous clasp designs,” Dentistry Today, 31(10):138-141.
Google Scholar
11) Kaufmann R, Friedli M, Hug S and Mericske-Stern R (2009) “Removable dentures with implant support in strategic positions followed for up to 8 years,” International Journal of Prosthodontics, 22(3):233-241.
Google Scholar
12) Kunwarjeet Singh, Himanshu Aeran, Narender Kumar and Nidhi Gupta (2013) “ Flexible Thermoplastic Denture Base Materials for Aesthetical Removable Partial Denture Framework,” Journal of Clinical Diagnostic Research, 7(10): 2372—2373.
Google Scholar
13) Loe H and Silness J (1963) “Periodontal disease in pregnancy. Prevalence and severity,” Acta Odontologica Scandinavica, 21:533-551.
Google Scholar
14) Minoretti R, Triaca A and Saulacic N (2009) “The use of extraoral implants for distal-extension removable dentures: a clinical evaluation up to 8 years,” International Journal of Oral and Maxillofacial Implants, 24(6):1129-1137.
Google Scholar
15) Moussa A, Ramadan A, Zaki I, Yehia D, Zeid A and Wael A (2012) “Viscoelastic properties of Thermo-Elastic resin reline with different ratios,” Journal of Applied Sciences Research,8(3):1477-1483.
Google Scholar
16) Ohkubo C, Kobayashi M, Suzuki Y and Hosoi T (2008) “Effect of implant support on distal-extension removable partial dentures: in vivo assessment,” International Journal of Oral and Maxillofacial Implants, 23(6):1095-1101.
Google Scholar
17) Osada H, Shimpo H, Hayakawa T and Ohkubo C (2013) “Influence of thickness and undercut of thermoplastic resin clasps on retentive force,” Dental Materials Journal, 32(3):381-389.
Publisher – Google Scholar
18) Phoenix RD, Cagna DR and DeFreest CF (2008) Stewart’s clinical removable partial prosthodontics, 4th edition, Quintessence publishing Co. Inc., Chicago, USA.
Google Scholar
19) Singh K, Aeran H, Kumar N and Gupta N (2013) “Flexible Thermoplastic Denture Base Materials for Aesthetical Removable Partial Denture Framework,” Journal of Clinical Diagnostic Research, 7(10): 2372—2373.
Google Scholar
20) Sykes LM, Dullabh HD, Chandler HD, Bunn B and Essop AR (2002) “Flexibility of technopolymer clasps compared with cobalt-chromium and titanium clasps,” Journal of the South African Dental Association, 57(5):166-171.
Google Scholar
21) Tokue A, Hayakawa T and Ohkubo C (2013) “Fatigue resistance and retentive force of cast clasps treated by shot peening,” Journal of Prosthodontic Research, 57 (3):186-194.
Publisher – Google Scholar
22) Turkyilmaz I (2009) “Use of distal implants to support and increase retention of a removable partial denture: a case report,” Journal of the Canadian Dental Association, 75(9):655-658.
Google Scholar
23) Yu H and Huang W (2012) “Category design and clinical application of esthetic clasps,” Hua Xi Kou Qiang Yi Xue Za Zhi, 30(5):447-452.
Google Scholar